- Apa saja struktur yang merupakan bagian dari anatomi genitalia wanita?
- Apa yang terjadi dalam siklus menstruasi?
- Berapa jumlah sel telur yang dimiliki oleh seorang wanita?
Sistem reproduksi wanita dirancang untuk sejumlah fungsi :
- Menghasilkan sel telur atau oosit yang diperlukan dalam proses reproduksi
- Sarana transportasi sel telur menuju tempat fertilisasi
- Tempat terjadinya fertilisasi di tuba falopii
- Tempat implantasi hasil fertilisasi di uterus sebagai awal proses kehamilan
- Ovarium menghasilkan hormon seksual wanita yang perlu bagi fungsi reproduksi
Bila tidak terjadi fertilisasi dan atau implantasi maka sistem reproduksi akan mengalami proses menstruasi ( pelepasan mukosa uterus setiap bulan )
Selama menopause produksi hormon seksual dari sistem reproduksi wanita yang penting bagi berlangsungnya siklus reproduksi secara bertahap akan berkurang. Bila seorang wanita sudah berhenti menghasilkan hormon seksual maka wanita tersebut sudah mengalami menopause.
Apa saja struktur yang merupakan bagian dari anatomi organ reproduksi wanita?
Anatomi reproduksi wanita terdiri dari struktur eksternal dan struktur internal.
Peran struktur eksternal :
- Jalan masuk sperma kedalam tubuh wanita
- Melindungi organ genitalia interna dari serangan infeksi mikiro organisme
Struktur Eksternal Sistem Reproduksi Wanita :
- Labia majora: Labia Major menutup dan melindungi sejumlah struktur eksternal. Struktur ini homolog dengan skrotum pria. Labia major memiliki kelenjar lemak dan kelenjar keringat. Setelah pubertas labia major tertutup dengan rambut pubis.
- Labia minora: Labia major panjangnya kira kira 5 sentimeter dan terletak didalam labia major dan mengitari orifisium vaginae dan meatus urethrae eksternus.
- Kelenjar Bartholin: Kelenjar ini terletak disamping orifisium vaginae dan memproduksi cairan encer (mukus).
- Klitoris: Labia minor kiri dan kanan bertemu dibagian anterior didaerah klitoris , satu tonjolan kecil yang homolog dengan penis pada pria. Klitoris terutup lipatan kulit yang disebut preputium yang juga terdapat pada pria. Seperti halnya penis, klitoris adalah struktur erektil yang peka terhadap rangsangan
Struktur Internal Sistem Reproduksi Wanita :
- Vagina: Vagina adalah saluran yang menghubungkan servik ( bagian terbawah uterus ) dengan bagian luar tubuh dan dikenal pula sebagai jalan lahir.
- Uterus (womb): Uterus adalah organ berbentuk seperti buah peer yang memiliki rongga untuk tempat pertumbuhan dan perkembangan janin. Uterus terbagi menjadi dua bagian : servik uteri dan corpus uteri yang akan menampung janin selama kehamilan. Servik memiliki saluran didalamnya yang disebut sebagai kanalis servikalis yang berperan sebagai saluran masuk sperma dan saluran keluar darah haid
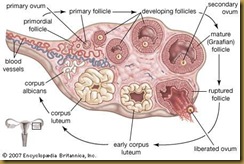
- Ovariums: Ovarium adalah dua buah kelenjar berbentuk bulat lonjong dan pipih yang terdapat disamping uterus. Ovarium menghasilkan sel telur dan hormon seksual wanita.
- Tuba Falopii: Saluran yang berada di bagian atas uterus kiri dan kanan yang berperan sebagai saluran ovarium untuk perjalanan sel telur dari ovarium ke uterus. Konsepsi , fertilisasi sel telur oleh sperma terjadi dalam tuba falopii dan selanjutnya hasil fertilisasi akan menuju ke uterus dan mengalami implantasi kedalam endometrium.
Apa yang terjadi dalam siklus menstruasi?
Wanita pada usia reproduksi akan mengalami aktivitas hormonal siklis yang berulang setiap bulan. Pada setiap siklus, tubuh wanita yang berada pada masa reproduksi mempersiapkan diri menghadapi kemungkinan terjadinya kehamilan. Istilah menstruasi.merujuk pada peristiwa peluruhan berkala dari endometrium ( Menstru artinya “ setiap bulan” dan dari sinilah awal munculnya istilah siklus menstruasi )
Siklus menstruasi rata rata berlangsung setiap 28 hari dan berlangsung dalam fase folikuler, ovulasi dan fase luteal.
Terdapat 4 hormon utama yang secara langsung mempengaruhi jalannya siklus menstruasi :
- FSH – Follicle Stimulating Hormone
- LH – Luteinizing Hormone
- Estrogen
- Progesteron
GnRH – Gonadotropin Releasing Hormone adalah hormon hipotalamus yang berperan memicu pengeluaran FSH dan LH dari hipofisis.
Fase Folikuler
Fase ini dimulai sejak hari pertama siklus haid. Selama fase folikuler siklus haid terjadi serangkaian peristiwa sebagai berikut :
- FSH dan LH dilepaskan dari hipofisis dan menuju ke ovarium melalui aliran darah
- FSH merangsang pertumbuhan dan perkembangan 15 – 20 sel folikel primer dalam ovarium
- FSH dan LH berperan pula dalam memicu pelepasan estrogen dari ovarium
- Dengan peningkatan kadar estrogen dalam darah maka produksi FSH akan menurun, mekanisme ini berfungsi untuk membatasi agar tidak terjadi pertumbuhan dan perkambangan folikel primer lebih lanjut.
- Dengan berlanjutnya fase folikuler, satu diantara sejumlah folikel yang tumbuh dan berkembang akan mengalami pertumbuhan dan perkembangan yang dominan sampai tahap matur. Pertumbuhan folikel yang dominan ini akan menekan pertumbuhan dan perkembangan folikel lainnya sehingga berhenti dan mati. Sel telur dominan ini akan terus memproduksi estrogen.
- Pada saat ini, endometrium akan tumbuh dan disebut stadium proliferasi
Ovulasi
Dalam siklus menstruasi 28 hari, fase ovulasi atau ovulasi terjadi 14 hari setelah awal fase folikuler. Fase ovulasi kurang lebih berada pada pertengahan siklus menstruasi dsan fase menstruasi akan terjadi sekitar 14 hari pasca ovulasi.
Selama fase ini terjadi serangkaian kejadian sebagai berikut :
- Meningkatnya estrogen dari folikel yang dominan merupakan pemicu keluarnya sejumlah hormon LH
- Hormon LH akan menyebabkan terjadinya ovulasi
- Setelah ovulasi, sel telur akan ditangkap oleh fimbriae dan dibawa kedalam tuba falopii
- Pada fase ini, lendir servik semakin banyak dan kental yang berguna untuk menangkap sperma dan memberi makan sperma sehingga mampu bergerak kedepan agar terjadi fertilisasi
Fase Luteal
Fase luteal dimulai sejak ovulasi dan meliputi sejumlah proses bagai berikut :
- Setelah melepaskan sel telur, folikel kosong akan menjadi struktur baru yang disebut corpus luteum
- Corpus luteum akan menghasilkan progesteron yang berperan lebih lanjut dalam mempersiapkan uterus agar hasil fertilisasi dapat mengalami proses implatasi
- Pada stadium ini, endometrium akan terus tumbuh dan disebut stadium sekresi
- Bila terjadi fertilisasi sperma atas sel telur maka embrio akan berjalan dalam tuba falopii menuju ke uterus dan mengadakan implantasi
- Bila tidak terjadi fertilsasi, sel telur akan terus berjalan menuju uterus . Oleh karena tidak diperlukan untuk mendukung kehamilan maka endometrium akan luruh dan terjadilah haid.
Berapa jumlah sel telur yang dimiliki oleh wanita?
Sebagian besar sel telur dalam ovarium akan mengalami kematian dan hilang saat seorang wanita mengalami menopause.
Pada saat lahir, neonatus diperkirakan memiliki 1 juta sel telur , jumlah tersebut terus menurun dan saat pubertas hanya tersisa sekitar 300.000.
Sepanjang masa reproduksi, terdapat sekitar 300 – 400 sel telur yang tumbuh matang dan mengalami ovulasi.